Diabetic Retinopathy
This article has been written to help people with diabetic retinopathy and their families and friends better
understand the disease. It describes the cause, symptoms, diagnosis, and treatment of diabetic retinopathy.
Diabetic retinopathy is a potentially blinding complication of diabetes that damages the eye's retina. It affects half
of all Americans diagnosed with diabetes.
At first, you may notice no changes in your vision. But don't let diabetic retinopathy fool you. It could get worse
over the years and threaten your good vision. With timely treatment, 90 percent of those with advanced diabetic
retinopathy can be saved from going blind.
The National Eye Institute (NEI) is the Federal government's lead agency for vision research. The NEI urges all
people with diabetes to have an eye examination through dilated pupils at least once a year.
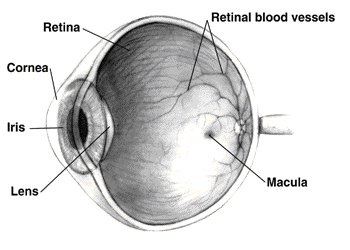
The retina is a light-sensitive tissue at the
back of the eye. When light enters the eye,
the retina changes the light into nerve
signals. The retina then sends these signals
along the optic nerve to the brain. Without a
retina, the eye cannot communicate with the
brain, making vision impossible.
people do not notice any changes in their vision.
Some people develop a condition called macular edema. It occurs when the damaged blood vessels leak fluid
and lipids onto the macula, the part of the retina that lets us see detail. The fluid makes the macula swell,
blurring vision.
As the disease progresses, it enters its advanced, or proliferative, stage. Fragile, new blood vessels grow
along the retina and in the clear, gel-like vitreous that fills the inside of the eye. Without timely treatment, these
new blood vessels can bleed, cloud vision, and destroy the retina.
Who is at risk for this disease?
All people with diabetes are at risk--those with Type I diabetes (juvenile onset) and those with Type II diabetes
(adult onset). During pregnancy, diabetic retinopathy may also be a problem for women with diabetes. It is
recommended that all pregnant women with diabetes have dilated eye examinations each trimester to protect
their vision.
What are its symptoms?
Diabetic retinopathy often has no early warning signs. At some point, though, you may have macular edema. It
blurs vision, making it hard to do things like read and drive. In some cases, your vision will get better or worse
during the day.
View of boys by person with normal vision. View of boys by person with diabetic retinopathy.
this happens it may not be very severe. In most cases, it will leave just a few specks of blood, or spots, floating
in your vision. They often go away after a few hours.
These spots are often followed within a few days or weeks by a much greater leakage of blood. The blood will
blur your vision. In extreme cases, a person will only be able to tell light from dark in that eye. It may take the
blood anywhere from a few days to months or even years to clear from the inside of your eye. In some cases,
the blood will not clear. You should be aware that large hemorrhages tend to happen more than once, often
during sleep.
How is it detected?
Diabetic retinopathy is detected during an eye examination that includes:
Visual acuity test: This eye chart test measures how well you see at various distances.
Pupil dilation: The eye care professional places drops into the eye to widen the pupil. This allows him or her
to see more of the retina and look for signs of diabetic retinopathy. After the examination, close-up vision may
remain blurred for several hours.
Ophthalmoscopy: This is an examination of the retina in which the eye care professional: (1) looks through a
device with a special magnifying lens that provides a narrow view of the retina, or (2) wearing a headset with a
bright light, looks through a special magnifying glass and gains a wide view of the retina.
Tonometry: A standard test that determines the fluid pressure inside the eye. Elevated pressure is a possible
sign of glaucoma, another common eye problem in people with diabetes.
Your eye care professional will look at your retina for early signs of the disease, such as: (1) leaking blood
vessels, (2) retinal swelling, such as macular edema, (3) pale, fatty deposits on the retina--signs of leaking
blood vessels, (4) damaged nerve tissue, and (5) any changes in the blood vessels.
Should your doctor suspect that you need treatment for macular edema, he or she may ask you to have a test
called fluorescein angiography.
In this test, a special dye is injected into your arm. Pictures are then taken as the dye passes through the
blood vessels in the retina. This test allows your doctor to find the leaking blood vessels.
How is it treated?
There are two treatments for diabetic retinopathy. They are very effective in reducing vision loss from this
disease. In fact, even people with advanced retinopathy have a 90 percent chance of keeping their vision when
they get treatment before the retina is severely damaged.
These two treatments are laser surgery and vitrectomy. It is important to note that although these treatments
are very successful, they do not cure diabetic retinopathy.
Laser Surgery
Laser surgery is performed in a doctor's office or eye clinic. Before the surgery, your ophthalmologist will: (1)
dilate your pupil and (2) apply drops to numb the eye. In some cases, the doctor also may numb the area
behind the eye to prevent any discomfort.
The lights in the office will be dim. As you sit facing the laser machine, your doctor will hold a special lens to
your eye. During the procedure, you may see flashes of light. These flashes may eventually create a stinging
sensation that makes you feel a little uncomfortable.
You may leave the office once the treatment is done, but you will need someone to drive you home. Because
your pupils will remain dilated for a few hours, you also should bring a pair of sunglasses.
For the rest of the day, your vision will probably be a little blurry. If your eye hurts a bit, your eye care
professional can suggest a way to control this.

Macular Edema: Timely laser surgery can reduce vision loss from macular edema by half. But you may need
to have laser surgery more than once to control the leaking fluid.
During the surgery, your doctor will aim a high-energy beam of light directly onto the damaged blood vessels.
This is called focal laser treatment. This seals the vessels and stops them from leaking. Generally, laser
surgery is used to stabilize vision, not necessarily to improve it.
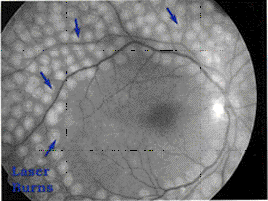
Proliferative Retinopathy: In treating advanced diabetic retinopathy, doctors use the laser to destroy the
abnormal blood vessels that form at the back of the eye.
Scatter laser treatment.
Once you have proliferative retinopathy, you will always be at risk for new bleeding. This means you may need
treatment more than once to protect your sight.
Vitrectomy
Instead of laser surgery, you may need an eye operation called a vitrectomy to restore your sight. A vitrectomy
is performed if you have a lot of blood in the vitreous. It involves removing the cloudy vitreous and replacing it
with a salt solution. Because the vitreous is mostly water, you will notice no change between the salt solution
and the normal vitreous.
Studies show that people who have a vitrectomy soon after a large hemorrhage are more likely to protect their
vision than someone who waits to have the operation.
Early vitrectomy is especially effective in people with insulin-dependent diabetes, who may be at greater risk of
blindness from a hemorrhage into the eye.
Vitrectomy is often done under local anesthesia. This means that you will be awake during the operation. The
doctor makes a tiny incision in the sclera, or white of the eye. Next, a small instrument is placed into the eye. It
removes the vitreous and inserts the salt solution into the eye.
You may be able to return home soon after the vitrectomy. Or, you may be asked to stay in the hospital
overnight. Your eye will be red and sensitive. After the operation, you will need to wear an eyepatch for a few
days or weeks to protect the eye. You will also need to use medicated eye drops to protect against infection.
What research is being done?
The NEI is currently supporting a number of research studies in both the laboratory and with patients to learn
more about the cause of diabetic retinopathy. This research should provide better ways to detect, treat, and
prevent vision loss in people with diabetes.
For example, it is likely that in the coming years researchers will develop drugs that turn off enzyme activity that
has been shown to cause diabetic retinopathy. Some day, these drugs will help people to control the disease
and reduce the need for laser surgery.
What can you do to protect your vision?
The NEI urges all people with diabetes to have an eye examination through dilated pupils at least once a year.
If you have more serious retinopathy, you may need to have a dilated eye examination more often.
A recent study, the Diabetes Control and Complications Trial (DCCT), showed that better control of blood
sugar levels slows the onset and progression of retinopathy and lessens the need for laser surgery for severe
retinopathy.
The study found that the group that tried to keep their blood sugar levels as close to normal as possible, had
much less eye, kidney, and nerve disease. This level of blood sugar control may not be best for everyone,
including some elderly patients, children under 13, or people with heart disease. So ask your doctor if this
program is right for you.
© Copyright 1999 Dialog Medical, Inc. All rights reserved.